The Community Acquired Pneumonia guideline implements parts of the Infectious Diseases Society of America, Practice Guidelines for the Management of Community-Acquired Pneumonia in Adults, updated by the 2003 Update of Practice Guidelines for the Management of Community-Acquired Pneumonia in Immunocompetent Adults. See also Community-acquired pneumonia in adults: guidelines for management. (1998) . In the SAGE Project, we fully implemented triage and non-ICU inpatient treatment. We also worked on order sets for Ambulatory treatment, ICU treatment, and Hospital Discharge.
All the details of the encoding in Protégé for Community Acquired Pneumonia have been generated as a web page [click here].
This guideline exemplar uses 180 Criteria in 5 Recommendation Sets with 18 Decision Nodes, 13 Context Nodes, and 45 Action Nodes.
This PowerPoint Presentation shows a typical patient presenting in an emergency room, with the SAGE CAP guideline in action: [ppt].
| Scenarios | Vocabulary | Logic |  top top |
|
|||
- SCENARIO: Outpatient with Fever, Chills, and Productive Cough
-
An adult patient presents to the outpatient clinic or emergency room with fever, chills and a productive cough. Blood work and a Chest X-ray are done and a diagnosis of Pneumonia is made. SAGE detects the new problem on the Problem List. Using the Pneumonia Severity Index (PSI) (Agency for Healthcare Research and Quality. Rockville, MD.), a recommendation is made for the clinicians regarding outpatient, or non-ICU or ICU inpatient therapy.
A specific order set is generated for each patient, with orders and groups of orders pre-selected, and annotated for the situation for each patient. Our order set is modeled using the newly proposed HL7 Standard for Order Sets. For inpatients, it includes sections for each of
- Admission, Discharge, and Transfer
- Consults
- Vital Signs Assessment
- Diet
- Activity
- Laboratory
- Ancillary
- Treatments
- Education
- IV Fluids
- Medications
The XML form of this order set is shown here [xml]. This same order set has been used in the HL7 ballot process (xml). It has evolved for that process somewhat beyond our usage in the project.
In addition, items from the JCAHO Pneumonia Core Measure Set are supported by inquiries to the clinical staff and monitoring of antibiotic and blood culture timing are performed along with reminders for getting those done on time.
Examples:
- The guideline specifically supports Measure PN-3b [pdf] which checks on whether blood cultures are done before antibiotics are administered in the hospital.
- The SAGE Engine monitors the inpatient record for blood cultures and antibiotic administration to support adherence to JCAHO measures PN-5ab [pdf].
| Scenarios | Vocabulary | Logic |  top top |
|
|||
Here are examples of the standard terminology used in this guideline, organized by Virtual Medical Record (VMR) class. In each class, there will be terms of different types. For example, to describe an allergic reaction, one needs the allergen, the type of reaction, and the severity of that reaction. Here we see codes from SNOMED Clinical Terms (SNOMED CT), and Logical Observation Identifiers Names and Codes (LOINC®), NDF-RT, and International Classification of Diseases, Ninth Revision (ICD-9).
The project maintains SAGE-defined concepts in separate SAGE terminologies that are linked to existing standard terminologies if the SAGE concept is either derived from or should be an addition to the external standard. For example if a SAGE concept was defined as a collection of LOINC concepts, it is maintained as a member of the SAGE LOINC terminology. If a concept's intent is consist with a particular terminology's intent, such as SNOMED CT and is a reasonable candidate for inclusion in a future release, it is maintained in the appropriate SAGE-linked terminology, such as SAGE SNOMED CT.
The concepts listed here are examples of the coded values used in each of the Virtual Medical Record classes. They are NOT examples of the class instances themselves. For example, Adverse Reactions requires a substance, like B-lactam, and a reaction type like Anaphylaxis. So, both concepts would show up under Adverse Reaction.
The CAP Guideline uses 265 concepts:
| VMR Class | Number of Concepts |
|---|---|
| AdverseReaction | 4 |
| Encounter | 1 |
| MedicationOrder | 7 |
| Observation | 57 |
| Problem | 183 |
| Procedure | 1 |
| SubstanceAdministration | 4 |
| VMROrder | 8 |
- AdverseReaction 4 of 4
- ERYTHROMYCINS/MACROLIDES [NDF-RT C8742]
- CAP-focused B-lactam [SAGE NDF-RT C88]
- CAP-focused respiratory fluroquinalone [SAGE NDF-RT C89]
- Allergic drug reaction (disorder) [SNOMED CT 74069000]
- Encounter 1 of 1
- Inpatient stay (finding) [SNOMED CT 308540004]
- Medication Order 5 of 7
- WARFARIN SODIUM PREPARATION [NDF-RT C21528]
- ERYTHROMYCINS/MACROLIDES [NDF-RT C8742]
- Class Ia antiarrhythmics [SAGE NDF-RT C114]
- CAP-focused respiratory fluroquinalone [SAGE NDF-RT C89]
- Antibacterial drugs (product) [SNOMED CT 346325008]
- Observation 8 of 57
- PH:SCNC:PT:BLDA:QN: [LOINC 2744-1]
- BODY TEMPERATURE:TEMP:PT:^PATIENT:QN: [LOINC 8310-5]
- HEART BEAT:NRAT:PT:XXX:QN: [LOINC 8867-4]
- Oxygen saturation measurement (procedure) [SNOMED CT 104847001]
- Bronchopneumonia, organism unspecified [ICD-9-CM 485]
- UREA NITROGEN:MCNC:PT:BLD:QN: [LOINC 6299-2]
- Class II CAP risk [SAGE C77]
- Systolic Blood Pressure [SNOMED CT 271649006]
- Problem 5 of 183
- Neoplastic Disease That Affect Pneumonia Risk [SAGE SNOMED CT C1]
- Prolonged QT Interval [SNOMED CT 111975006]
- Raynaud's Disease [SNOMED CT 195295006]
- Wide QRS Ventricular Tachycardia [SNOMED CT 251156000]
- Renal Artery Stenosis [SNOMED CT 302233006]
- Procedure 1 of 1
- Hysterectomy [SNOMED CT 236886002]
- SubstanceAdministration 4 of 4
- ERYTHROMYCINS/MACROLIDES [NDF-RT C8742]
- CAP-focused B-lactam [SAGE NDF-RT C88]
- CAP-focused Respiratory Fluroquinalone [SAGE NDF-RT C89]
- Antibacterial Drugs [SNOMED CT 346325008]
- VMROrder 5 of 8
- referral to smoking cessation advisor [SNOMED CT 395700008]
- Analysis of Arterial Blood Gases and pH [SNOMED CT 60170009]
- mechanical regular diet [SNOMED CT 63740007]
- Blood Culture, Active Status (C100) [SNOMED CT 30088009]
- Blood Culture, Completed Status (C101) [SNOMED CT 30088009]
| Scenarios | Vocabulary | Logic |  top top |
|
|||
Top Level Logic for Community Acquired Pneumonia |
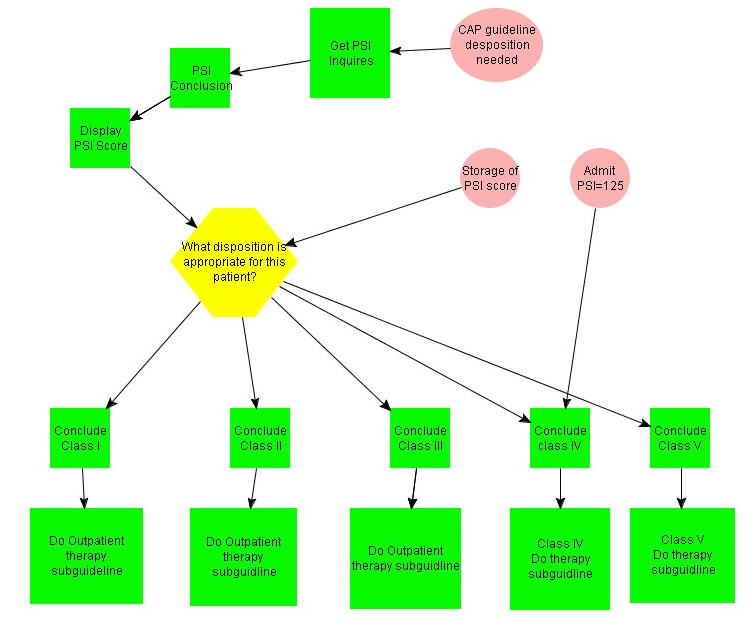
The guideline starts when the problem of Pneumonia is added to a patient's Problem List, or when a new Pneumonia Severity Index value is recorded. In the Protégé recommendation set below there is a single decision node "What disposition is needed for this patient?" from which 5 alternative treatment action sets derive. This recommendation set also has a test Context for setting the PSI Score to 125 for Class IV Pneumonia. This was used in testing our inpatient Non-ICU scenario.
Pneumonia Severity Index (PSI) |
|
The PSI score is computed using 18 observations, if they are available. The input screen below shows those observations along with SAGE's assessment as to the right answer (TRUE or FALSE) in each case for a particular patient. In this case, Roger Dogeman (not a real patient) has a BUN of 34, and an O2 Saturation of 88%. There was no evidence in the record of any of the other conditions contributing to the PSI score: Neoplastic disease, Liver disease, etc.

The PSI score is computed using a GELLO expression. The formula is available inside the guideline to support recomputation should a physician wish to use the calculator in a test mode, or to try alternative values if observations are uncertain. Each of the ?variables has a value of 1 (true) or 0(false). Roger Dogeman's score was 98, putting him in the Class IV triage category, requiring Inpatient Non-ICU treatment.
((?Age.divide(1000*60*60*24*365))-10*(?Female))+ (10*(?NHomeStatus))+ (30*(?NeoplasticDis))+ (10*(?CVDisease))+ (20*(?CLDisease))+ (10*(?CRDisease))+ (10*(?CHF))+ (10*(?BUN))+ (10*(?Glucose))+ (20*(?Sodium))+ (10*(?Hematocrit))+ (30*(?ArtPH))+ (20*(?RR))+ (20*(?SBP))+ (20*(?ALTMental))+ (10*(?Pulse))+ (15*(?Temp))+ (10*(?O2Sat))+ (10*(?BilPleuE))
Outpatient Therapy |
|
For outpatients, the logic adjusts and annotates the orders for treatment and follow-up without admission. See the encoded guideline HTML output format here. The outpatient order set has been designed but has not yet been added to the encoding.
Inpatient Therapy |
|
Both Class IV and Class V patients use the same inpatient recommendation set. It has a context node with two outgoing pathways. Both are executed in parallel.
The upper action node ("Record JCAHO-specific measures") asks the clinician for specific JCAHO measurement information. Some of these can be determined from the record. Those values will be shown if they are available. The measures are:
- Is the Pneumococcal Vaccine up to date?
- Is the Influenza Vaccine up to date?
- Is there risk for Pseudomonas?
- Transferred from an outside ED?
- Previous antibiotics for this episode of CAP?
- Blood cultures obtained prior to arrival?
- Will this patient have comfort measures only?
- Is there risk for Pseudomonas?
All of the answers to the JCAHO questions above can be used in annotating the order set for this patient. For example, a known risk of Pseudomonas will pre-select a different antibiotic regime.
Depending, then, on whether this patient is Class IV or Class V, then regular Non-ICU treatment, or ICU treatment is followed respectively. In both cases, Admission Order Sets are recommended.

Order Sets |
|
The contents of the Inpatient Order Set were mentioned above. Here is a web page version of the Order Set for a particular Class IV patient. Notice the pre-selection (radio buttons and choices) of items and groups or items, the XOR and AND logic connecting order items, and the (bold) text annotation that SAGE generates for particular orders.
Shown here is the annotated Medications section of the Order Set.

Critical Actions |
|
After the Admitting orders have been recommended, three items are monitored by the guideline. They are
- whether blood cultures have been drawn,
- whether O2 Saturation or Arterial Blood Gases have been measured, and
- whether antibiotics have been administered.
Shown here is the Blood Culture portion of the Critical Action recommendation set which looks for all three activities and wakes itself up with a self-generated event "Generate CAP monitoring Event", to look again if the items have not been completed. This part determines if the cultures have been drawn, and if not whether there is an existing order for them. It alerts the team either to order the cultures, or to get the test done in a timely way. SAGE stops looking for the cultures when it determines that they have been drawn. This recommendation set exits through the context node "Patient's Blood culture was drawn".
There is very similar logic for both the ABGs and for the Antibiotics.


 Scenarios
Scenarios